Chest osteochondrosis is a degenerative-dystrophic chronic process of damage to the intervertebral discs and vertebral bodies of the thoracic spine. This disease is slightly less common than osteochondrosis of the cervical or lumbosacral spine. However, this does not mean that it does not cause trouble for the person. Osteochondrosis of the thoracic spine is manifested mainly by pain in the back and chest, but can also give pain in the heart, abdomen, similar to angina pectoris or hepatic colic. In rare cases, osteochondrosis of the thoracic spine causes the development of paresis of the muscles of the lower extremities, impaired sensitivity in them, disorders of the pelvic organs. The treatment of the disease consists in the use of medical and non-medical methods, and sometimes even surgery is required. In this article you will learn about the symptoms that manifest osteochondrosis of the thoracic spine, and methods for its treatment.
Thoracic spine
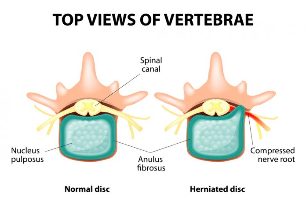
The thoracic spine is represented by 12 vertebrae, between the bodies of which there are intervertebral discs. The discs consist of nucleus pulposus and annular fibrosis. Pathological changes in these discs, as well as in the adjacent facet joints, growth of bone spines at the edges of the vertebral bodies, dystrophic processes in the ligaments of the spine and become a direct cause of back pain.
It should be understood that osteochondrosis as a disease rarely affects only one part of the spine. Usually this process is diffuse, more or less pronounced in different parts of the spine.
Some structural features of the thoracic spine lead to the fact that it is less often affected by osteochondrosis than other regions of the spine. Let's list these features:
- less mobility of the thoracic spine;
- the presence of vertebral joints with ribs (which in combination with the sternum creates a strong chest frame, less susceptible to injury);
- small thickness of the intervertebral discs;
- physiological kyphosis (bending in the anterior-posterior direction with a protrusion directed backwards) of the thorax and therefore the maximum axial load falls on the anterior rather than the posterior sections of the discs.
Another characteristic not of the structure but of the development of osteochondrosis of the thoracic spine, which determines the lower frequency of pain in the thoracic spine, is that the existing morphological bases of osteochondrosis in this part mayremain clinically "dull" for a long time. That is, there are changes, but they do not bother the patient.
However, in the presence of provoking factors, such as a sedentary lifestyle (including years of working at a desk or driving a car), injuries, poor posture, relaxed back muscles, heavy physical labor in a forced position, osteochondrosis of the chesta basket on the spine shows its true face.
Symptoms of osteochondrosis of the thoracic spine
The main clinical symptom of osteochondrosis of the chest, as well as other parts, is pain. Back pain, chest pain, even pain in the internal organs. In medicine, it is common to distinguish several pain syndromes (and not only pain) of osteochondrosis of the thoracic spine. In general, they are divided into two groups:
- reflex;
- compression.
Reflex syndromes are clinical manifestations of spinal receptor stimulation. These are receptors for connections, capsules of intervertebral joints, intervertebral discs, which receive pathological impulses in osteochondrosis. In addition to pain, reflex syndromes may be accompanied by muscle tension, autonomic disorders in soft tissues and internal organs. Such changes are based on the following fact: stimulation of the receptors leads to the spread of excitation in the nearby structures of the spinal cord (more precisely to the segments of the spinal cord). And these can be neurons responsible for the sweating of a particular area of the skin, regulating the temperature of the same area, involved in ensuring the activity of internal organs (heart, liver, intestines, etc. ), maintaining muscle tone and blood circulationvessels that supply all these structures. And when excitation is transmitted to these neurons, there are corresponding symptoms of dysfunction of certain formations. Therefore, such a situation is quite possible when the pain in the abdomen or in the heart area is caused by osteochondrosis of the chest.
Compression syndromes occur when the nerve root is compressed (rarely stretched), when it leaves the intervertebral foramen, spinal cord tissue or the vessels that feed it. Compression syndromes are almost always caused by an existing disc herniation. The most common are hernias of the lower thoracic segments. Depending on the direction and location of the hernia, a person experiences certain symptoms. This can be represented as follows:
- Median (median) hernias are accompanied by the development of muscle weakness symmetrically in both legs, loss of sensitivity in them. At the same time, the pain syndrome typical of nerve root compression is absent;
- lateral (lateral) hernias show extreme pain associated with nerve root compression;
- medio-lateral hernias combine the clinical symptoms of the two previous groups, with only muscle weakness and sensory disturbances predominating on the convex disc side.
What type of syndromes are considered within osteochondrosis of the chest? Let's talk in more detail about the types of reflex and compression syndromes at this level.
Reflex syndromes
Dorsago- acute sudden pain in the thoracic spine. It has an acute nature, often described by patients as a dagger blow. It is generally felt between the shoulder blades, can be given to the heart, sternum. Patients are afraid to move and even take a deep breath because the pain intensifies (as if it fires again). Quite often these symptoms appear after a long stay in a fixed awkward position while doing monotonous work. Sudden movement then provokes dorsago in people with osteochondrosis of the thoracic spine. Palpation of the thoracic spine reveals tension in the paravertebral muscles in the form of a roller and their soreness.
Sometimes such pain can be seen as a heart attack, so strong and sudden it seems to the patient. However, the electrocardiogram taken has no abnormalities and the use of nitroglycerin under the tongue does not eliminate the pain.
Dorsalgiais another type of chest reflex syndrome. This is a pain syndrome that occurs gradually. The pain can be localized in any part of the back, chest. Painfully painful, dull, sometimes with a hint of burning (which is associated with irritation of vegetative structures). It is intensified by movements of the spine, bending, rotating around its axis, coughing or sneezing, driving on uneven roads.
Pain may be felt in the intercostal spaces on one or both sides. This characteristic is due to the course of the nerve conductors (intercostal nerves and vessels are located in the intercostal space). In this case, the pain is called intercostal neuralgia, by analogy with shingles pain.
If the pain is localized to the anterior chest wall, it is also called pectalgia. However, it can only be felt in some places with an intact back. For example, in the area of the xiphoid process or at the site of attachment of the sternocleidomastoid muscle. Quite often, due to the painful and dull nature of the pain, it is difficult to understand exactly where it hurts: either something inside the chest or in the area of the superficial soft tissues.
Dorsalgia may be accompanied by reflex tension of the paravertebral muscles, more pronounced on the pain side. In this case, of course, the muscle tension is not as pronounced as in a similar situation in the lumbar spine. However, on palpation, muscle tightness is felt and the touch itself causes discomfort or pain. It is also painful to palpate the interspinal spaces and paravertebral points in the area of the segment affected by osteochondrosis.
Reflex syndromes in osteochondrosis of the chest are much more common than compression.
Compression syndromes
Nerve root compressionis accompanied primarily by pain syndrome. Pain is shooting in nature. The direction of pain distribution corresponds to the course of nerve fibers. In the case of thoracic osteochondrosis, these are the intercostal spaces. Because some of the nerve fibers form plexuses involved in the innervation of internal organs, pain can be felt inside the chest, abdomen. The pain intensifies when moving, tilting the body, coughing, sneezing, laughing (because in these moments the tension of the root increases). In the area that the compressed root innervates, sensitivity disorders can be observed: a feeling of crawling, tingling, numbness. Touching this area may not feel good. In cases where the nerve root is subjected to compression for a long time, motor disorders can occur, ie the weakness of the muscles that it innervates. The muscles gradually atrophy. However, movement disorders are very rare, as they are the latest in the chronology of the onset of all symptoms. Usually a person seeks medical help at the stage of pain and sensory disturbances.
Compression of the spinal cordmanifests as weakness in the legs with a simultaneous increase in muscle tone (if the spinal cord is compressed in the lower thoracic spine, muscle tone decreases). Pathological symptoms of the legs may occur (Babinsky et al. ). Sensitivity in the lower extremities is lost, the sensation of touching cold and hot does not differ, the difference between just touching and injecting. In cases of severe spinal cord compression, urinary incontinence may occur.
The compression of the blood vessels that feeds the spinal cord leads to the development of myeloischaemia, ie malnutrition of the spinal cord tissue. This, as well as spinal cord compression, is accompanied by the development of muscle weakness (patients say "legs have refused"), loss of sensation and pelvic disorders.
It is fair to say that compression of the spinal cord and its vessels in thoracic osteochondrosis is very, very rare.
Vegetative components of osteochondrosis of the thoracic spine

Due to the fact that the nerve fibers coming from the thoracic spine contain autonomous conductors, irritation or disruption of these fibers may be accompanied by autonomic symptoms. These can be:
- dryness and peeling of the skin in the area of innervation of a single nerve;
- local violation of sweating and thermoregulation (also according to the zone of innervation);
- coldness of the lower limbs, brittle toenails;
- pain simulating diseases of the gastrointestinal tract (eg, gastritis, gastric ulcer, cholecystitis, etc. );
- pain in the kidneys, which actually has nothing to do with kidney pathology (no changes in urine and ultrasound);
- pain in the heart, very similar to angina pectoris and even myocardial infarction.
The peculiarity of such pain may be the fact that a person may not feel back pain. This is initially misleading for both the patient and the medical staff when seeking medical help. However, performing a number of additional methods of examination makes it possible to exclude the pathology of the internal organs and then osteochondrosis of the chest is considered the cause of such pain.
Treatment of osteochondrosis of the thoracic spine
All methods of treating osteochondrosis of the chest are divided into medical and non-medicinal. In most cases, only a combination of the two groups has an effect and the disease subsides. Although you need to understand that it is simply impossible to completely get rid of osteochondrosis of the chest. The degenerative process can be stopped, slowed down, but there is no reversal.
Medicine
The main directions of drug exposure in osteochondrosis of the chest are elimination of pain, elimination of muscle tension, improvement of microcirculation and tissue trophism.
Non-steroidal anti-inflammatory drugs have been used successfully to relieve pain syndrome. Drugs in this group have the ability to reduce the inflammatory process, eliminate pain and block platelet aggregation. The drugs are prescribed for an average of 7-14 days. This is usually enough to eliminate the pain. Many of them are available in different forms (tablets, capsules, injectable solutions, rectal suppositories), which ensures easy use. In the first days of treatment, the drugs are used in injectable form, and then switched to tablets or suppositories. The same drugs can be used topically at the same time: on the thoracic spine. In addition, for this purpose there are various forms of release: creams, ointments, gels, plasters.
Sometimes non-steroidal anti-inflammatory drugs are not enough to relieve pain. In such cases, resort to the use of analgesic mixtures. The mixtures are injected intravenously into saline or glucose.
Paravertebral block has a very good and fast analgesic effect. This is a type of medical manipulation when a drug is injected near the spine intradermally, subcutaneously, into the thickness of the muscle tissue, perineurally (directly near the nerve or root). The procedure requires certain skills and experience of the doctor.
Topically, irritating and distracting ointments can be used to reduce the pain of osteochondrosis of the thoracic spine. These are ointments containing snake venom, bee venom and pepper extracts.
Muscle tension is relieved by non-drug methods.
Diuretics, hormones, Escina Lysinat are used to relieve nerve root swelling.
Pentoxifylline, dipyridamole, complamin, nicotinic acid are used to normalize blood circulation, improve tissue nutrition and restore trophism.In osteochondrosis of the thoracic spine, B vitamins are shown to have analgesic and neurotrophic effects.
When exacerbation of osteochondrosis of the thoracic spine, you can resort to the use of drugs that improve the metabolism of the intervertebral discs and joints. These are the so-called chondroprotectors. These drugs stimulate the regeneration of articular cartilage, stop the degenerative process in the intervertebral discs. They are prescribed for a long time (3-6 months).
Non-drug methods
These include:
- massage (classical, point, reflex-segmental);
- physiotherapy exercises;
- stretching of spasmodic muscles (there are special techniques, stretching is not done on the principle "as you want");
- acupuncture;
- swimming (very useful for all patients with any localization of osteochondrosis);
- physiotherapy (ultrasound, electrophoresis, amplipulse, diadynamic currents, mud therapy and so on).
If the hernia resulting from osteochondrosis of the thoracic spine compresses the spinal cord, its vessels or nerve roots and at the same time causes muscle weakness, pelvic dysfunction, severe pain syndrome (drug-resistant)), then the issue is considered for surgical treatment.
Osteochondrosis of the thoracic spine is not a deadly disease, but it causes a lot of harm to a sick person. It limits his life, interferes with work and good rest. The main symptom of osteochondrosis of the chest is pain. It is impossible to completely get rid of this disease, but it is possible to stop the degenerative process and minimize its manifestations.





































